Урология №2 / 2023
Оценка характера назначения лекарственных препаратов при гиперактивном мочевом пузыре специалистами различных специальностей в Индии: анализ тенденций в назначениях
1) Технологический университет Гуджарата, Ахмадабад, Индия;
2) Институт управления бизнесом «Симбиоз», Пуна, Махараштра, Индия;
3) Международный журнал диабета и эндокринологии, Ахмадабад, Гуджарат, Индия;
4) Отделение анестезиологии, Институт медицинских наук и исследований им. Сардара Валлаббхаи Пателя, Эллис бридж, Ахмадабад, Гуджарат, Индия
Цель: оценить характер назначения лекарственных препаратов при гиперактивном мочевом пузыре специалистами различного профиля в Индии.
Материалы и методы: проанализированы результаты вторичного аудита по продажам (Quintiles and IMS Health), а также аудита назначения антимускариновых препаратов и агониста бета-3-адренорецепторов (мирабегрона) с 2014 по 2021 г. Аудит проводился для оценки тенденций в использовании солифенацина, оксибутинина, толтеродина, дарифенацина, троспия и мирабегрона представителями различных специальностей; кроме того, проанализированы назначения урологами солифенацина и мирабегрона.
Результаты: урологи выписали 65% препаратов для лечения ГАМП в 2016 г. и 54% в 2021 г. Среди других специалистов, чаще всего в 2021 г. выписывали препараты хирурги (11%), гинекологи (9%) и врачи-консультанты (8%). Кроме того, 100% назначенных лекарств в 2016 г. составили антимускариновые средства (мирабегрон – 0%), а в 2021 г. на их долю пришлось 58% (мирабегрон – 42%). Самым частым антимускариновым препаратом был солифенацин, далее оксибутинин, толтеродин, дарифенацин и троспий. В 2016 г. препараты для лечения ГАМП выписывали 38% урологов, а в 2021 г. – 33%. Только солифенацин назначали 748 урологов в 2018 г. и 739 в 2021 г., а мирабегрон – 961 и 934 соответственно. Ежегодная динамика в количестве назначений за последние 6 лет (с 2016 по 2021 г.) для солифенацина и мирабегрона составила -3% и 8% соответственно.
Заключение: урология по-прежнему чаще всего назначают препараты для лечения ГАМП, хотя их также выписывают хирурги и врачи-консультанты. Отмечается тенденция к назначению вместо антимускариновых препаратов бета-агониста мирабегрона. На основании результатов данного исследования специалисты станут чаще использовать лекарственную терапию при ГАМП, что приведет к более эффективному оказанию помощи.
Introduction. There are a variety of symptoms associated with an overactive bladder (OAB), which include urgency, frequency, and nocturia, with or without urge urinary incontinence (UUI)[1]. OAB is also associated with decreased quality of life and a high economic cost to society [2].
International Continence Society (ICS) estimates that 12.8% of women and 10.8% of men suffer from OAB; the prevalence of frequency, urgency, and urge incontinence (UI) rises with age [3, 4]. Men’s UUI was significantly lower than women’s. There is a 10–42% prevalence in India, with a progressive increase in prevalence from the third to seventh decade of life (5.6%, 14.2%, 27.3%, 34.3%, and 39%, respectively) [5].
Behavioral and self-control training and other OAB treatment methods are regarded as first-line options for reducing urine incontinence in patients. Antimuscarinics or β3 adrenoceptor agonists are popular treatments for OAB if behavioral changes fail to alleviate symptoms [6]. Some of India’s most commonly prescribed OAB medications among antimuscarinics are solifenacin, oxybutynin, tolterodine, darifenacin, trospium and mirabegron and among anti-adrenoceptor agonists, mirabegron is most common (Table 1) [7].
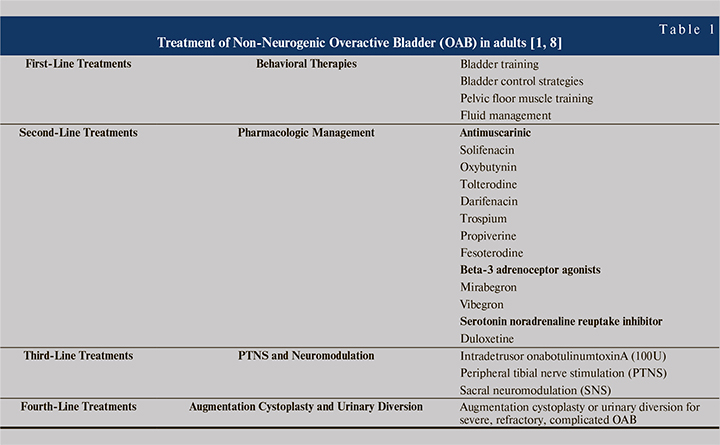
Antimuscarinics prevent the contraction of the smooth muscle wall around the bladder. Stimulation of the acetylcholine muscarinic M3 receptors in the detrusor muscle wall usually results in micturition. Solifenacin and darifenacin are muscarinic receptor antagonists that only affect the M3 receptor. Oxybutynin and tolterodine are non-selective antimuscarinics that affect all muscarinic receptors, which causes dry mouth [9]. As a beta-3 agonist, mirabegron relaxes the detrusor muscles and enhances bladder storage capacity without affecting voiding contractions. As a result, mirabegron can assist in alleviating the symptoms of OAB [10]. According to a report by the Urological Society of India, OAB is most commonly treated with antimuscarinic or beta-3 adrenoceptor agonists. Most patients with stress urine incontinence turn to the serotonin noradrenaline reuptake inhibitor duloxetine [5, 11].
The objective of the present study is to assess the prescribing practices for OAB pharmacotherapy especially antimuscarinic and beta-3 adrenoceptor agonists, based on the prescription trend analysis across different specialties of India. Moreover, we expect that the accumulation of data from this study will eventually lead to evidence-based medicine that can lead to more advanced OAB treatments irrespective of medical specialties.
Materials and Methods. Data source and setting. From August 2016 to August 2021, we have been using IQVIA Medical Audit Data (formerly IMS Health) to track the urological preparation (G04B) prescription rates for primary care physicians in India who work in the private sector [12]. In more than 100 countries, IQVIA, a non-profit organization, collects market intelligence and disseminates it. Medical audit data monitor prescriptions written by allopathic doctors in private practices. Data were gathered from a random sample of 4600 healthcare practitioners from 23 metropolitan areas of India (over 1 million population), 128 Class 1 cities (population over 100,000), and 1A cities (population fewer than 100,000). A national sample of prescriptions written by doctors in cities with populations greater than one million was drawn from the original data [13].
The data use the European Pharmaceutical Market Research Association’s (EphMRA) anatomical therapeutic classification (ATC), not the World Health Organization’s (WHO) ATC classification. The diagnoses reported on prescriptions are also not coded for the International Classification of Diseases and Related Health Problems (ICD-10). In addition, because the data does not include prescriptions written in the public sector, our analysis only includes outpatient prescription samples from that sector. Last but not least, IQVIA makes the data available to us in aggregate form, processed, and extrapolated to reflect national prescription practices.
Outcome measure. Study focused on the number of antimuscarinic and mirabegron prescribed each year as a primary outcome measure. In addition, study estimated and reported prescriptions by specialty and molecule. For each molecule, number prescribers or their specialties were evaluated.
Statistical analysis. Study used the International Statistical Classification of Diseases and Related Health Problems, 10th Revision, to code prescription diagnosis data from an IQVIA medical audit (ICD-10 classification; version: 2016) [13]. Anatomic Therapeutic Chemical (ATC) classification of antimuscarinics and beta-3 adrenoceptor agonists recommended for the related diagnosis have been coded to the 3rd level of WHOCC’s proposed drug statistics methodology (ATC index-2016) [14]. By searching an online index using keywords in the diagnosis given in the medical audit data, taken directly from the prescription, the diagnosis was assig...